
How Do Gums Heal After Tooth Extraction?
Have you been advised to get a tooth extracted and are wondering what comes next? Tooth extraction is a common dental procedure, followed by a
The team at Albany Dental can treat gum disease, sleep apnea, teeth grinding and more.
Visit our Gosford clinic today to resolve your dental issue!



Have you been advised to get a tooth extracted and are wondering what comes next? Tooth extraction is a common dental procedure, followed by a

The latest in our 5 minute chat series is here! We find out what our staff love about the Central Coast and of course, Albany

The latest in our 5 minute chat series is here! We find out what our staff love about the Central Coast and of course, Albany

The latest in our 5 minute chat series is here! We find out what our staff love about the Central Coast and of course, Albany

When it comes to oral health, there’s a lot beneath the surface that many of us might not consider in our daily routines. But have

When it comes to restoring your smile, choosing the right type of dental crown is important. In this blog, we’ll explore different types of dental

Dental crowns offer more than just a cosmetic fix—they are important for restoring damaged teeth to their former strength and functionality. However, the question of

The latest in our 5 minute chat series is here! We find out what our staff love about the Central Coast and of course, Albany

The latest in our 5 minute chat series is here! We find out what our staff love about the Central Coast and of course, Albany

Fluoride: it’s in our toothpaste and often in conversations about our dental health. Yet, for something so common, its true story remains overshadowed by several
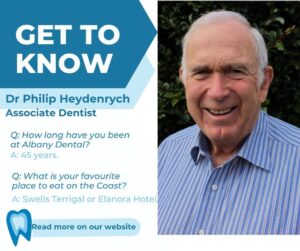
The latest in our 5 minute chat series is here! We find out what our staff love about the Central Coast and of course, Albany

The latest in our 5 minute chat series is here! We find out what our staff love about the Central Coast and of course, Albany
| Monday | 8:30am – 6:30pm |
| Tuesday | 8:30am – 5:30pm |
| Wednesday | 8:30am – 6pm |
| Thursday | 8:30am – 5pm |
| Friday | 8:30am – 3pm |
| Saturday | Closed |
| Sunday | Closed |
Contact Us
